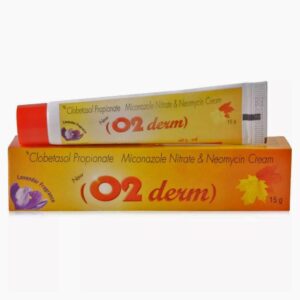
NEOMYCIN + MICONAZOLE + CLOBETASOL
Neomycin: Neomycin is an aminoglycoside antibiotic used to prevent or treat infections caused by bacteria. It is commonly used as a topical ointment or cream to treat minor skin infections, and also in oral or intravenous forms to treat gastrointestinal infections.
The mechanism of action of neomycin involves inhibiting bacterial protein synthesis. It binds to the 30S subunit of the bacterial ribosome, preventing the synthesis of essential proteins required for bacterial growth and survival.
The dosage of neomycin varies depending on the route of administration and the specific condition being treated. When used topically, a thin layer is typically applied to the affected area 2-4 times daily. For gastrointestinal infections, oral neomycin is generally taken every 6-8 hours for a period of 5-7 days. The dosage for intravenous administration is determined by the prescribing physician or healthcare provider.
As with any medication, neomycin can cause side effects. When used topically, it may cause skin irritation, redness, or itching. In rare cases, it can lead to an allergic reaction characterized by a rash, hives, or difficulty breathing. When taken orally or intravenously, neomycin can have more serious side effects, including kidney damage, hearing loss, and nerve damage. It is important to follow the prescribed dosage and duration of treatment to minimize the risk of these side effects.
Neomycin should be used with caution in individuals with pre-existing kidney or hearing problems, as they may be more susceptible to its adverse effects. It is also important to inform your healthcare provider about any other medications you are taking, as they may interact with neomycin.
Overall, neomycin is a commonly used antibiotic that is effective against a range of bacterial infections. However, it should be used judiciously and under the guidance of a healthcare professional to minimize the risk of side effects.
Miconazole: Miconazole is an antifungal medication used to treat various fungal infections. It is available in various formulations, including cream, powder, spray, and oral gel.
The mechanism of action of miconazole involves inhibiting the synthesis of ergosterol, a vital component of fungal cell membranes. By disrupting the production of this compound, miconazole weakens and eventually kills the fungal cells, thus treating the infection.
The dosage and duration of treatment with miconazole may vary depending on the type and severity of the infection. It is important to follow the instructions provided by a healthcare professional or the product label.
Miconazole may cause some common side effects, including skin irritation, itching, and burning at the site of application. These side effects are usually mild and temporary. In some cases, individuals may experience an allergic reaction to miconazole, manifesting as rash, hives, swelling of the face, lips, tongue, or throat, or difficulty breathing. It is important to seek immediate medical attention if any allergic reactions occur.
Other less common but more severe side effects may include blistering, peeling, or severe itching of the skin. If these occur, medical attention should be sought.
Some drug interactions are possible with miconazole. It is important to inform a healthcare professional about all medications, including over-the-counter drugs, vitamins, and supplements, to avoid any potential interactions.
It is recommended to consult a healthcare professional before using miconazole, especially if pregnant, breastfeeding, or have any underlying medical conditions.
Clobetasol: Clobetasol is a potent corticosteroid drug that is primarily used in the treatment of various skin conditions. It belongs to the group of drugs known as glucocorticoids.
The main use of Clobetasol is to relieve symptoms such as inflammation, redness, and itching associated with certain skin disorders like eczema, psoriasis, dermatitis, and allergic reactions. It can also be utilized in the treatment of other conditions, such as lichen planus and lupus erythematosus.
The mechanism of action of Clobetasol involves its ability to bind to the glucocorticoid receptors in the skin cells. By doing so, it modifies the production and activity of various inflammatory substances, such as prostaglandins and leukotrienes, which are responsible for triggering inflammation. This ultimately helps to reduce inflammation, redness, and itching in the affected areas.
Clobetasol is available in various forms including creams, ointments, lotions, and solutions. The dosage form and strength will depend on the specific condition being treated. It is usually applied topically on the affected area of skin once or twice daily, as directed by a healthcare professional. It is important to follow the prescribed dosage and duration of use to avoid excessive absorption or side effects.
While Clobetasol is an effective treatment option, it does come with potential side effects. Common side effects may include skin irritation, burning, stinging, dryness, or redness at the application site. Prolonged or excessive use of Clobetasol can also lead to skin thinning, stretch marks, and increased susceptibility to infections. In rare cases, systemic absorption can occur, leading to adrenal suppression, Cushing’s syndrome, and other systemic side effects.
It is important to consult with a healthcare professional before using Clobetasol. They will evaluate your specific condition and provide appropriate guidance on the dosage, duration of treatment, and precautions to minimize side effects and optimize the therapeutic benefits.