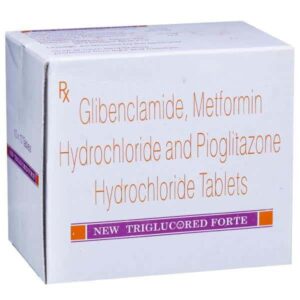
GLIBENCLAMIDE + METFORMIN + PIOGLITAZONE
Glibenclamide: Glibenclamide, also known as glyburide, is an oral antidiabetic drug belonging to the class of sulfonylureas. It is primarily used in the treatment of type 2 diabetes mellitus when diet and exercise alone is not sufficient to control blood sugar levels.
The mechanism of action of glibenclamide involves stimulating the release of insulin from the pancreatic beta cells. It binds to specific receptors on the beta cell membrane, which leads to depolarization of the cell and subsequent opening of calcium channels. This influx of calcium triggers the release of insulin into the bloodstream, thus lowering blood sugar levels.
The initial dose of glibenclamide is typically 2.5-5 mg, taken once daily with breakfast or the first main meal of the day. However, the dosage may vary depending on the patient’s response and blood sugar levels. The maximum recommended daily dose is 20 mg.
As with any medication, glibenclamide can cause certain side effects. Common side effects include hypoglycemia (low blood sugar levels), weight gain, nausea, stomach upset, increased sensitivity to sunlight, and rash. These side effects are usually mild and temporary. However, serious side effects can occur, such as allergic reactions, liver problems, and hematologic abnormalities. It is important to contact a healthcare professional if any unusual or severe side effects are experienced.
Glibenclamide should be used with caution in certain individuals, such as pregnant women, individuals with impaired liver or kidney function, and those with known sulfonylurea allergies. It is also contraindicated in patients with type 1 diabetes, diabetic ketoacidosis, and severe kidney or liver disease.
Overall, glibenclamide is an effective medication for the management of type 2 diabetes mellitus. However, it is important to follow the prescribed dose and to regularly monitor blood sugar levels to minimize the risk of adverse effects and ensure optimal control of diabetes.
Metformin: Metformin is a medication used to treat type 2 diabetes. It is also sometimes prescribed for individuals with prediabetes, gestational diabetes, and polycystic ovary syndrome (PCOS). Metformin is available in various forms, including tablets and extended-release tablets.
The mechanism of action of metformin involves reducing the amount of glucose produced by the liver and increasing the sensitivity of muscles and fat cells to insulin. This helps to lower blood sugar levels and improve insulin resistance. Metformin also has some effects on inhibiting the absorption of glucose from the intestines.
The typical starting dose of metformin is 500 mg once or twice a day, with meals. The dose may be gradually increased over time based on blood sugar levels and individual response, up to a maximum daily dose of 2,000 to 2,550 mg. Extended-release tablets are usually taken once daily with the evening meal.
Common side effects of metformin include gastrointestinal issues, such as nausea, diarrhea, and stomach upset. These side effects are often temporary and may improve as the body adjusts to the medication. Other less common side effects include lactic acidosis (a serious condition that can be fatal), vitamin B12 deficiency, and a metallic taste in the mouth.
It is important to note that metformin should not be used in individuals with severe kidney impairment or other conditions that can increase the risk of lactic acidosis. Regular monitoring of kidney function and blood sugar levels is recommended while taking metformin.
As with any medication, it is essential to consult a healthcare professional for personalized advice, dosage instructions, and possible interactions with other medications or conditions.
Pioglitazone: Pioglitazone is a medication used to treat type 2 diabetes mellitus. It is sold under the brand name Actos.
Mechanism of Action:
Pioglitazone belongs to a class of drugs called thiazolidinediones. It works by increasing the body’s sensitivity to insulin, a hormone that helps control blood sugar levels. Pioglitazone acts as an agonist for peroxisome proliferator-activated receptors (PPAR-gamma), which are found in adipose tissue, muscle, and the liver. Activation of these receptors helps improve insulin sensitivity, leading to better glucose utilization and regulation.
Use:
Pioglitazone is used to control blood sugar levels in patients with type 2 diabetes. It is often prescribed as part of a comprehensive treatment plan which includes diet, exercise, and other anti-diabetic medications. It can be used alone or in combination with other oral hypoglycemic agents such as metformin or sulfonylureas.
Dose:
The typical starting dose of pioglitazone is 15-30 mg once daily, which can be increased to a maximum of 45 mg per day if necessary. It is usually taken with or without food. The dosage may vary based on individual patient factors, and it is important to follow the instructions of the prescribing healthcare provider.
Side Effects:
Common side effects of pioglitazone include:
1. Weight gain – due to fluid retention and increased adipose tissue.
2. Edema – swelling in the ankles, feet, or hands.
3. Headache.
4. Upper respiratory tract infection.
5. Muscle pain.
6. Hypoglycemia – especially when combined with other diabetic medications.
Rare but serious side effects may include heart failure, liver problems, and bladder cancer. Pioglitazone may also increase the risk of fractures, particularly in women.
It is important to note that pioglitazone may not be suitable for everyone, especially those with a history of heart disease or bladder cancer. Therefore, it is crucial to consult with a healthcare professional before starting this medication.